The Role of Digital Platforms in Medication Adherence
Adherence to prescribed medications remains a significant challenge around the world. To combat this challenge in low- and middle-income countries, where the impacts of non-adherence can be particularly severe, global health organizations, Ministries of Health, and multilateral organizations have introduced Digital Adherence Technologies (DATs).
DATs are digital technologies that are intended to help support patients adhere to their medications by improving the consistency with which they take their medication. A function that all types of DATs have in common is the ability to generate a digital record of medication intake.
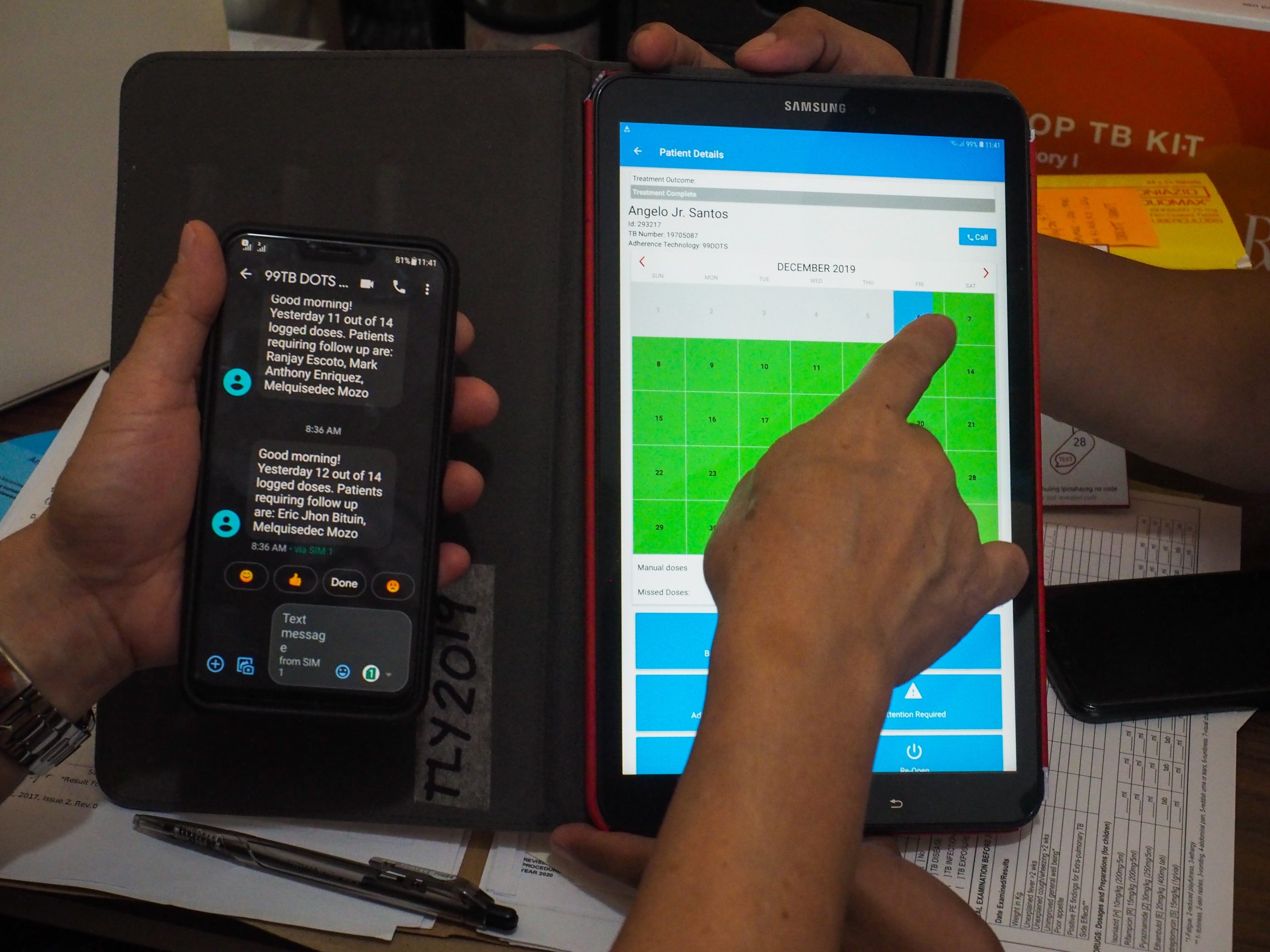
Typically, DATs relay adherence data to a “platform”, which aggregates this information, providing insights to the patient and/or healthcare provider about when and how often doses are taken or missed. These tools allow patients to take their medication at their convenience while remaining connected to healthcare workers, who use adherence data to determine when and how to follow-up with patients who miss doses.
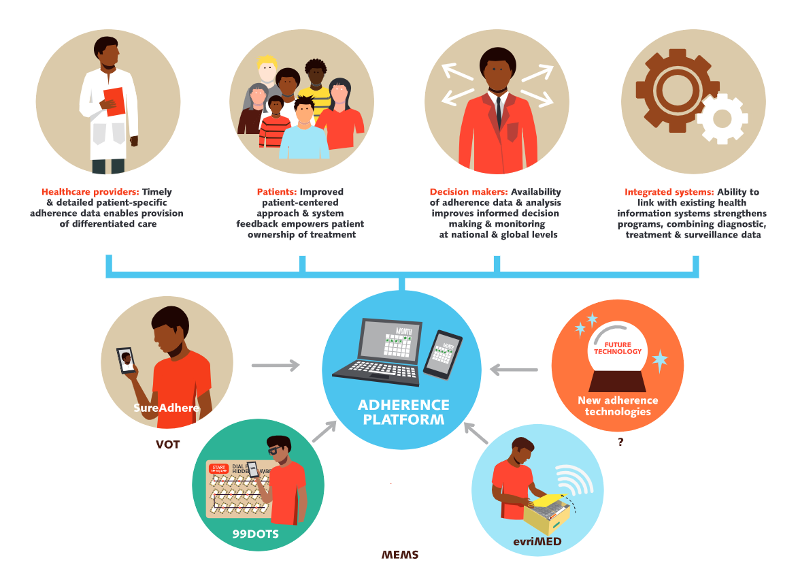
While there have been previous efforts to evaluate DATs themselves, far less attention has been paid to the platforms that aggregate and present DAT data for clinical decision making. Yet, these platforms are essential for DATs to function properly, creating a link between patient and provider.
This analysis focuses on the current state of the market for DAT platforms, including how they are being used, challenges to their effectiveness, enablers for successful utilization, and opportunities for the future.
1. Overview of Platform Categories
There are three main categories of DAT platforms currently serving the market and included in this.
> Developed to be used across a wide array of products, aggregating data from different sources and displaying adherence data that is device-agnostic.
> Particularly useful in a clinical setting where multiple types of adherence products are used within a single community – for instance, video-observed therapy (VOT) for those with smartphones, and smart pill boxes for those with feature phones.
> An example of this type of platform is the Everwell Hub, which is widely used for tuberculosis treatment in many countries.
> Packaged with a manufacturer-specific platform that is designed solely to be used with that device.
> In high-income countries, where DATs are often commercially available, this model is predominant.
> However, many DATs focused on LMICs also have attached platforms such as Wisepill Technologies, who offers a web management application for patient data and device tracking.
> Developed by country governments and civil society organizations.
> Governments may choose this option if they prefer to have more control over the system, see benefits from a cost or sustainability perspective, or have patient privacy concerns.
> A successful example of a country-led deployment is I LIKE VST, a mobile and web application built by Moldova’s Center for Health Policies and Analysis.
Where and how are platforms currently being used?
High-income Settings:
A major driver of DAT platform uptake in high-income countries are clinical trials, where it’s critical to understand whether a study participant has taken a medication under research. Platforms provide dashboards with participant dosing history, facilitating the identification of instances in which missed doses could influence research findings. For research trials, the primary users are clinical trial managers. This contrasts with another major use case in high-income countries, elder care for patients who have increased difficulty managing complex medication regimens. In this case, platforms can be patients, but also their families and care teams.
Low-and middle-income Settings:
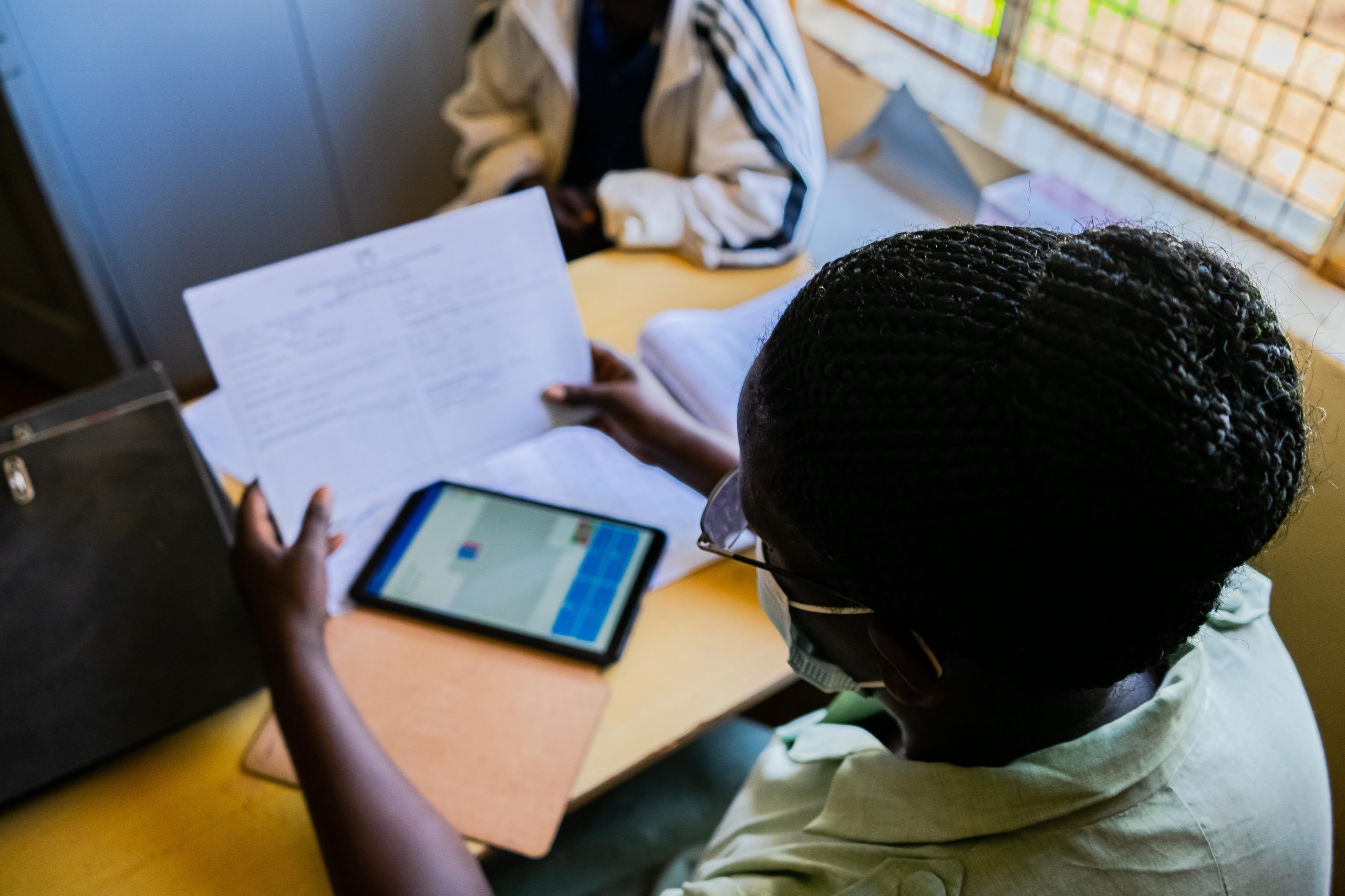
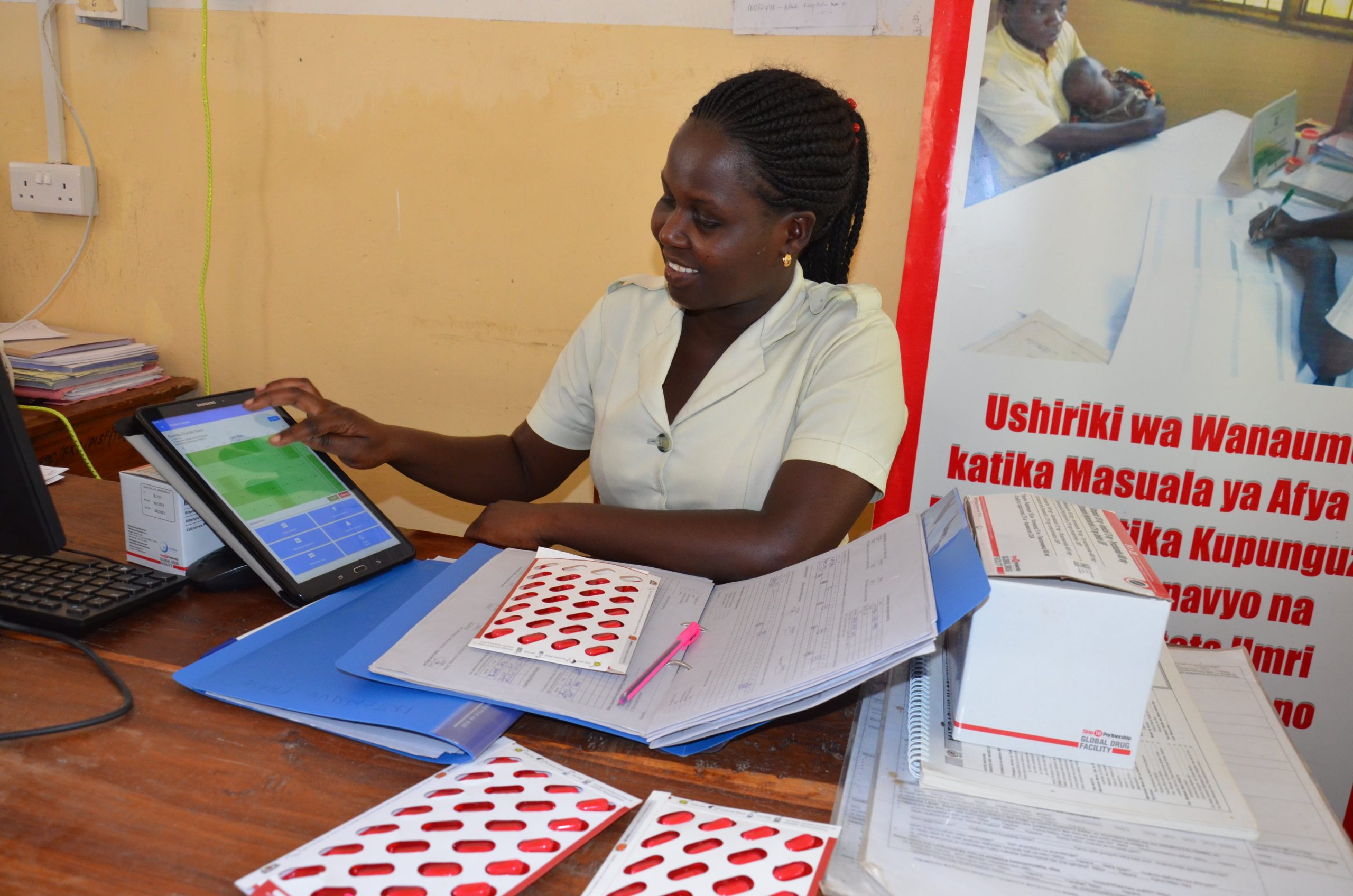
In low- and middle-income countries platforms are primarily used for patient adherence monitoring and support, currently. In many cases, this takes the form of an interface between patients and providers, enabling health care workers to visualize dosing histories, compile task lists and support actions for non-adherence patients, and send SMS reminders directly to those who require follow-up. Health workers are also using platforms in some geographies to monitor adverse reactions. In some countries, governments are evaluating the acceptability of digital adherence platforms, where research findings will inform policy makers on longer-term adoption.
How are platforms used?
Some platforms enable automated motivational messages to be sent to patients, enabling behavior change interventions. Another feature, which is aspirational for some platforms and being used in others, is utilizing machine learning to either evaluate the most effective messaging for patients or evaluate demographic risk factors based on adherence data.
Platforms also enable some health care workers to provide objective reporting to the broader health system or external organizations. For instance, in Moldova, implementing NGOs responsible for tuberculosis care are engaged on a pay-for-performance basis, utilizing data from platforms to measure and evaluate treatment adherence. In South Africa, providers generate statistical reports based on platform data when communicating regularly with the National TB Program on treatment adherence levels.
2. What’s working well?
“It’s easy because we can monitor the patients’ adherence wherever they are so we are able to see if they are taking their medication…. it is really working miraculously.” – Health Care Worker in South Africa
Digital adherence facilitated by platforms is widely seen as a vast improvement in areas where directly observed therapy was previously the standard of care.
From the health care worker’s perspective, platforms have dramatically decreased their workload in geographies as diverse as Philippines to Ethiopia, enabling providers to focus on patients that truly require their attention. In Moldova, DATs and related platforms have enabled providers to focus on COVID-19 patients by limiting the number of therapy observations needed. Instead, they only focus on those who need support. instead of engaging in time consuming therapy observation. Amid the current invasion of Ukraine, providers have been able to provide patients with a longer supply – of medication, monitoring and supporting them from afar, decreasing risks associated with traveling to the health facility for additional medication-. In the most extreme cases in Ukraine, providers who have evacuated active conflict zones where phone communication is impossible, have continued to track their patients via the platform, ensuring that they are still alive and well while also securing their own safety.
“Currently I use Everwell once per week to check doses and record them in eTB manager. Before the full-scale war in Ukraine started, either my colleagues or I used the platform at least once per day to check patients’ adherence.
If we noticed that someone didn’t take medicines, we called to those patients to find out what happened. Now I have evacuated, but the majority of our patients are still in Donetska oblast, some of them are on occupied territories. We could reach only a couple of them over the phone.
There were some patients who could not be reached over the phone, but then we noticed on the platform that they opened a box, so we could assume they were alive and safe.”
– Health Care Worker in Ukraine
Broadly, health care workers, donors, and government officials believe that patients are benefitting from these products as well. Many respondents reported that patients save money and reduce their health risks by communicating digitally over the platform with their providers rather than traveling to a clinic. Others consider platform mediated interactions to be a vast improvement in patient empowerment, allowing them more discretion over when and where they take their medication.
Respondents reported that among the characteristics working well for DAT platforms include:
✓ User friendly
✓ Convenient to use
✓ Asynchronous nature of adherence monitoring
✓ Include helpful visualizations on a dose-by-dose basis
✓ Provide reliable data
✓ Able to make real-time decisions
✓ Improve facility services
Currently, the Everwell Hub, which is an open-source platform that can be used on tablets, phones and desktops, is the only DAT platform on the market capable of incorporating data from multiple types and brands of technologies. The platform provides a “to do” list and adverse event reporting, facilitating regular tasks for providers. Importantly, the Everwell Hub can also generate reports and analytics in real time, enabling insights into overall adherence levels responsively. External organizations report that Everwell is open to continual learning and adapting the platform accordingly.
3. What’s not working well?
The challenge most cited was utilizing digital platforms effectively for medication adherence management was network coverage. Low levels of internet connectivity and electricity outages make it challenging for the platform systems to work effectively in real-time in many instances because they are operating without up-to-date adherence data.
Another common challenge is the human resources available to manage the back-end technology upkeep of a platform. There are concerns that not all health care workers have the technical capacity to manage digital platforms and some report difficulties interacting with the technology. Despite saving time and avoiding in-person interactions, in some cases platforms created additional complexity or work, particularly if the health care worker handles all programs and not just adherence-specific diseases.
Resourcing challenges are not limited to health care worker constraints. Resource challenges also abound if there is no dedicated funding to monitor patients through the platform, especially during COVID-19 when health budgets were reallocated and stretched thin. Others report that cost is a constant barrier for uptake, reporting that the use of DATs and digital platforms is far higher than the cost of the medication itself. Even if digital adherence solutions are cost-effective, governments are not accustomed to budgeting for this “extra” line item, which presents a challenge when asking NTPs to adopt and self- sustain the new technologies.
System challenges are also present in some cases. DAT platforms were not designed for WHO or NTP reporting, creating challenges when developing reports for these entities. In addition, there are multiple reports of platforms failing to respond at times, creating barriers to real-time use. Some homegrown platforms currently lack needed modules and some users worry about the confidentiality of the data.
Data entry and data quality are frequently noted challenges. For example, some DAT platforms do not accept Cyrillic alphabets, adding time and burden to health care workers who are then required to switch to Latin letters while inputting data. Others noted that the platform data is only as good as its inputs, with some patients triggering an adherence event while not taking medications, while others reported that their children opened Smart Pill Boxes leading to false reports.
4. What should the future direction of DAT platforms look like?
Business Models
There is little consensus on the right approach to developing effective business models to expand access to DATs and platforms. One respondent reported that there are no profitable business models that currently exist that fit into medical practice, and that even large pharmaceutical companies have found it difficult to make these products profitable in high income markets.
Another emerging theme is the challenge of fragmentation in the DAT platform market. A donor stressed that product-specific platforms have no role to play in the future of TB care in LMICs, which increases fragmentation within the market and makes integration across different DATs difficult. The number of platforms already on the market, including bespoke “homegrown” systems, have made it impossible to set standards for platform functionality across the market.
Countries, particularly in Eastern Europe and Southeast Asia, have chosen to build these homegrown systems to ensure sustainability and local ownership. This can cost as little as $30,000 – 40,000 and once it is built, it can be shared with other countries. For instance, Moldova has shared their homegrown system with Tajikistan and Uzbekistan, whose adoption of the platform has resulted in significant savings. A primary advantage to this model, according to those who have implemented it, is that it reduces ongoing costs to operate the system, which can be critical when grant financing ends. According to one respondent in sub-Saharan Africa, the only path to country-wide scale is transitioning ownership of DAT platforms to the Ministry of Health to enable full system integration.
Lastly, respondents pointed to grant funding cycles as a major challenge for DAT systems. A developer mentioned the perverse incentives to spend down grant funding to ensure future allocations, rather than reward cost-effectiveness/savings. Another respondent speculated that DAT systems may simply require long-term donor subsidization for a handful of countries with the highest TB burden.
Without Integration We Are “Washing One Baby a Hundred Times”
There is widespread recognition that integrating DAT platforms across DAT products and within larger digital health systems is critical for the ultimate success of digital adherence. According to one developer “The most important quality of a DAT platform is the flexibility to integrate with a lot of devices and the integration into other aspects of the healthcare system.”
Respondents in sub-Saharan Africa agreed, sharing that it would be important to integrate current DAT platforms into national systems, with one likening current system silos to “washing one baby a hundred times.” (SA) Beyond national systems generally, others pointed to the need to integrate digital adherence with screening, testing, treatment initiation and tracking of treatment outcomes.
One system that is pioneering unprecedented levels of integration across the cascade of patient care is Nikshay, a web enabled patient management system for TB control in India. With Nikshay, diagnosis, prescription, delivery of medication, and patients support for adherence are all packaged within a system, enabling incentives for patients for specific behavior. Nikshay provides a model for integrating adherence platforms within a larger digital system that could be replicated in other geographies.
While other countries may find it challenging to replicate Nikshay’s model, many countries use DHIS2 as a disease reporting tool, which could incorporate adherence data in the future.
Applications Beyond Tuberculosis
While DATs and platforms have had the widest uptake for tuberculosis in LMICs, there are many other potential indications that could benefit from adherence support. Among the disease areas that were mentioned by respondents were multiple suggestions for diabetes and HIV in South Africa and Ethiopia, maternal and pre-natal health, non-communicable diseases such as hypertension and mental health, as well as treatments that can influence TB outcomes, such as chronic disease management and cancer. There were also suggestions to view digital adherence from the perspective of the pharmaceutical space, examining and expanding to diseases and conditions that have a regular pill-taking component.
Functionality and Capacity Building
Based on experiences using DAT platforms, respondents have several suggestions on potential improvements for the future. From a functionality perspective, the platform could include features for patients to schedule appointments and organize visits rather than calling the personal phone number of a provider, which one health care worker suggested would improve patient workflows. Another respondent would like to see a patient-based application, rather than just a facility-based platform, with a patient/provider communication feature, enabling providers to ask questions about why doses were missed.

From a capacity standpoint, multiple respondents reported an interest in increased capacity building and training for health care workers regarding platform use. In some cases, these trainings are necessary due to high turnover rates of health care workers, requiring new providers to quick familiarize themselves with novel technologies and platforms.
| Editing function on the interface should be improved (13) | Philippines |
| Editable GREEN mark from adherent to missed dose (15) | |
| Potentially developing a new application that is specific for disease management or specifically for TB that is more user friendly. There might be too many functions within the current platform. (9) | Developer |
| Need to make the platform even more user-friendly (7) | |
| Customized flags for extremely delinquent patients missing three or more weeks of medications (7) | |
| Simplify the app for DATs to simplify the process of treatment monitoring for patients. (7) | Tanzania |
| Adding information in the system on other illnesses the patient has (chronic for example) and co morbidities. (7) |
Key Insights on DAT Platforms:
- Generally, DAT platforms are seen as very positive, reducing HCW burden, reducing disease exposure, etc. They are surprisingly helpful in unstable situations, maintaining connections to patients even when cell service goes out (Ukraine). Open-source platforms were largely praised for their flexibility to accept data from many DAT types.
- Platforms are only as good as the data that is put into them – network connectivity is a major barrier.
The Road Ahead:
- Not a lot of love for product-specific platforms in the future. In situations where cost or privacy is a large factor, homegrown systems appear to be a more favorable option
- Integration moving forward will be key – Widespread desire to incorporate platforms/adherence data in national-level systems like DHIS2
- Room to grow. Lots of stakeholders want to see platforms used across disease areas, not just TB
- Room to improve. Desired features include scheduling capability within the platform, better communication tools between patient/provider, and more capacity building from a tech perspective for HCWs
Credit
Information for this analysis was gathered July 2022. Initially, a rapid desk review assessment examined gap in current literature regarding DAT platforms. The desk review consisted of a google search and compiling of previous partner/project resources. Conversations (18 in total) were conducted virtually with donors, developers, health care workers and national TB program personnel who work with DAT platforms across 8 countries (Ethiopia, India, Moldova, Philippines, South Africa, United States).
KNCV and PATH would like to recognize the following organizations for their input and perspectives:
The Arcady Group, The Bill and Melinda Gates Foundation, Stop TB Partnership, Keheala, Moldova Ministry of Health, Aardex, Wisepill, Everwell, Tanzania National TB Program, Ukraine National TB Program, South Africa National TB Program, Philippines National TB Program, and Ethiopia National TB Program.